Clinical Cases
Diabetic Retinopathy Retina
What is Diabetic Retinopathy?
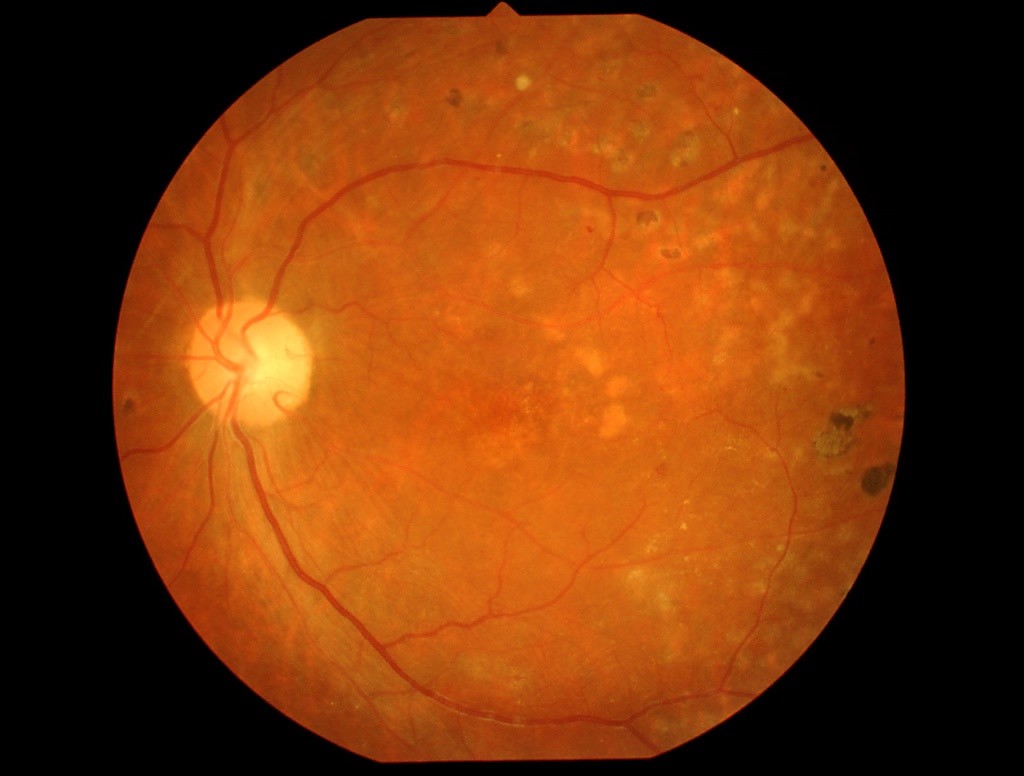
Diabetic Retinopathy is the leading cause of preventable blindness in the active population. It is estimated that diabetics are 25 times more likely to blind than the general population. Diabetic Macular Edema is one of the major complications, accounting for most cases of Diabetic Retinopathy with associated visual loss. It is associated with the presence of accumulated fluid in the central area of the retina (macula).
This pathology almost always evolves without visual symptoms, which may arise only in very advanced stages of the disease. Identifying patients at risk by allowing them to undergo therapeutic interventions in a timely manner represents the most important challenge for all health professionals involved.
Treatment of Diabetic Retinopathy
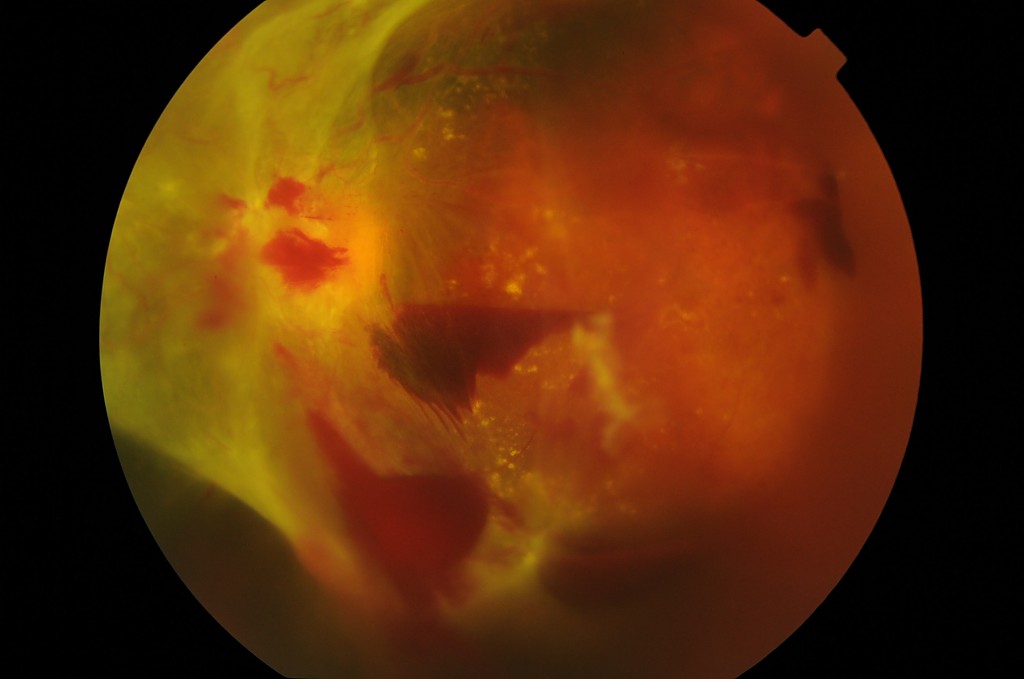
Most patients need only regular eye examinations, every six months or every year. In other cases, it is necessary to inject intravitreal medications (anti-VEGF and corticosteroids) and to selectively apply Laser to the abnormal vessels of the retina to reduce macular edema and ischemic areas (without blood supply) in order to prevent the progression of the disease. In the more advanced cases, with intravitreal (intraocular) hemorrhage and / or tractional retinal detachment, intraocular microsurgery (vitrectomy) should be performed.